Kidney Failure Stem Cell Therapy: Separating Clinical Reality from Marketing Claims
Kidney Failure Stem Cell Therapy: Separating Clinical Reality from Marketing Claims
The search for kidney failure stem cell therapy reflects a profound hope shared by millions of patients worldwide. With chronic kidney disease (CKD) affecting approximately 697.5 million people globally as of 2017 and projections indicating CKD will become the fifth leading cause of death by 2040, the desperation for breakthrough treatments is entirely understandable.
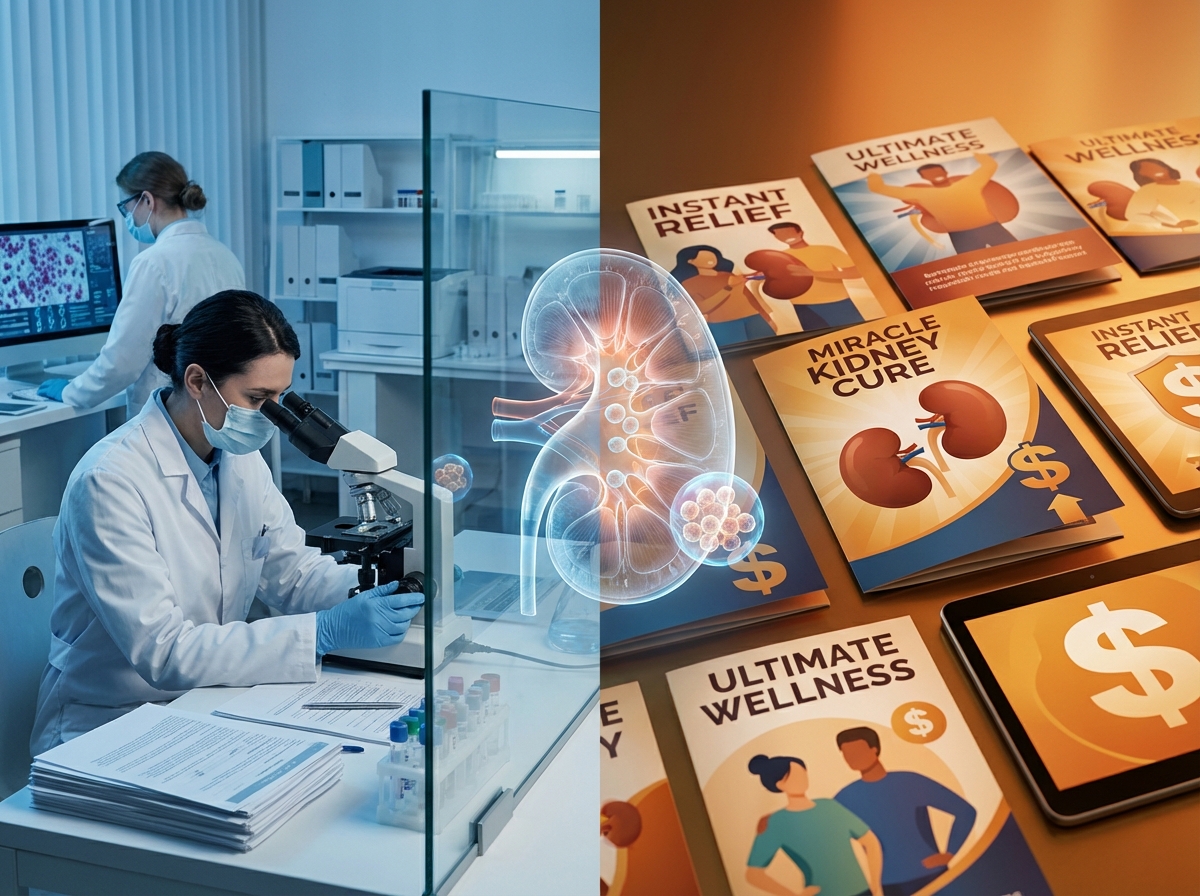
However, a significant gap exists between the aggressive marketing claims circulating online and the actual regulatory approval status of these treatments. As of 2026, zero FDA-approved stem cell treatments exist for kidney disease. This article provides an honest assessment of what is real, what remains experimental, and where the evidence currently stands.
The Current FDA Status of Stem Cell Therapy for Kidney Disease
Patients searching for kidney disease treatments must understand one critical fact: there are currently no FDA-approved stem cell treatments for kidney disease. The Harvard Stem Cell Institute confirms that while researchers are conducting clinical trials to test whether stem cell-based therapies are safe and effective, none have achieved approval status.
The term “experimental” carries significant implications. It means these treatments have not demonstrated sufficient safety and efficacy through rigorous clinical trials to warrant regulatory approval for commercial use. This distinction matters because patients paying for unapproved treatments assume substantial risk without the protection of proven outcomes.
The FDA has taken enforcement action against companies promoting stem cell therapies for kidney failure and other conditions without approval. Over the past year, the FDA sent 46 manufacturers and healthcare professionals regulatory correspondence, including warning letters. Additionally, the Federal Trade Commission secured a settlement requiring $525,000 to be returned to consumers who purchased treatments based on unsubstantiated claims.
Standard approved treatments remain dialysis—costing approximately $40,000 to $90,000 annually per patient depending on the payer and treatment type—and kidney transplantation. While these options present challenges, they represent proven interventions with established outcomes.
Understanding the Clinical Trial Landscape
The research landscape shows genuine scientific interest in stem cell applications for kidney disease. According to published research, more than 40 clinical trials involving stem cell therapy for kidney diseases were registered as of 2021, with most utilizing mesenchymal stem cells (MSCs).
However, “clinical trial” and “approved treatment” represent fundamentally different categories. Clinical trials test hypotheses under controlled conditions with extensive safety monitoring. Approved treatments have completed this process and demonstrated sufficient evidence of safety and efficacy.
Current legitimate research includes:
- UC Davis PROACT Study (2025): UC Davis Health launched an investigation of Renal Autologous Cell Therapy (REACT) for CKD caused by type 2 diabetes
- Mayo Clinic Research (October 2025): Mayo Clinic researchers found that fat-derived mesenchymal stem cells improved dialysis blood vessel healing in 21 participants
- Wake Forest Institute Findings: Wake Forest researchers demonstrated urine-derived stem cells showed promise in preclinical models with reduced scarring and inflammation
These represent research settings with strict protocols—not commercial treatments available to the general public.
Why Animal Studies Haven’t Translated to Human Success
One of the most significant challenges in kidney disease stem cell research involves the translation gap. Despite numerous animal experiments showing promising results, outcomes have not been successfully reproduced in human clinical studies.
Several factors contribute to this challenge:
Species-Specific Differences: Animal models, typically rodents, possess different physiological characteristics than humans. Their kidney structure, immune responses, and healing mechanisms do not perfectly mirror human biology.
Artificial vs. Natural Disease: Laboratory-induced kidney disease in animals differs substantially from the natural disease progression humans experience. Artificially created conditions may respond differently to treatment than diseases developing over years or decades.
Disease Complexity: Human kidney disease involves multiple contributing factors. Diabetes mellitus represents the leading global cause of CKD, followed by glomerulonephritis and hypertension. This complexity makes treatment more challenging than addressing a single induced condition.
Mechanism of Action: MSCs work primarily through paracrine mechanisms—releasing healing factors—rather than directly regenerating kidney tissue. This indirect mechanism makes predicting human outcomes from animal models particularly difficult.
Mixed Clinical Trial Results: What the Data Actually Shows
Clinical trial results reveal a nuanced picture rather than universal success or failure. According to published research, outcomes vary significantly by condition type:
- Lupus Nephritis: Stem cells have been used to treat lupus nephritis patients with good complete recovery rates
- Diabetic Nephropathy: Clinical trials using MSCs did not show sufficient therapeutic effect
- Acute Kidney Injury (AKI): Treatment effects remain controversial and disputed
A critical limitation involves disease staging. Treatments are primarily conducted at CKD stages 3 and 4. At stage 5—complete kidney failure with extensive fibrosis—regeneration to a functional state becomes unfeasible, making kidney transplantation necessary.
Red Flags: How to Identify Unproven Claims
Patients seeking treatment must learn to recognize warning signs of unproven or fraudulent claims:
Warning Sign #1: Clinics claiming to “cure” or “reverse” kidney disease without FDA approval should prompt immediate skepticism.
Warning Sign #2: Promoting international treatment options specifically to circumvent U.S. regulatory standards indicates potential problems.
Warning Sign #3: Relying on individual testimonials or case studies rather than systematic clinical trial data suggests insufficient evidence.
Warning Sign #4: Failing to distinguish between different kidney disease stages and treatment applicability demonstrates a lack of medical rigor.
Warning Sign #5: Not disclosing experimental status or lack of FDA approval prominently represents a significant ethical concern.
When evaluating any regenerative medicine claim, patients should verify FDA approval status, request peer-reviewed research supporting the treatment, and demand transparent discussion of limitations.
The Evidence Standard: How Rigorous Research Should Work
The FDA’s Cellular & Gene Therapy Products framework exists to protect patients from unsafe or ineffective treatments. Clinical trials progress through phases:
- Phase 1: Tests safety in small groups
- Phase 2: Evaluates effectiveness and side effects
- Phase 3: Confirms effectiveness in larger populations
- Phase 4: Monitors long-term effects after approval
This process requires controlled studies, peer review, and reproducible results. While the urgency patients feel is valid, patient safety demands this rigorous approach. Participating in legitimate clinical trials differs fundamentally from paying for unproven commercial treatments—the former advances science while protecting participants; the latter exploits hope without accountability.
Understanding Orthopedic Regenerative Medicine: Current Evidence and Limitations
While stem cell therapy is not approved for kidney disease, some patients may be exploring regenerative medicine for orthopedics for other conditions. Understanding the current regulatory landscape for these treatments is important.
According to the FDA, regenerative medicine therapies—including stem cell products—have not been approved for the treatment of any orthopedic condition, such as osteoarthritis, tendonitis, disc disease, tennis elbow, back pain, hip pain, knee pain, neck pain, or shoulder pain. The only FDA-approved stem cell products in the United States consist of blood-forming stem cells derived from umbilical cord blood for use in patients with disorders affecting blood production.
Some orthopedic applications of regenerative medicine, including PRP (platelet-rich plasma) therapy and certain autologous cell concentrates, may be offered under specific regulatory frameworks that do not require FDA approval when cells are minimally manipulated and used for homologous purposes. However, patients should understand that “not requiring FDA approval” differs from “being FDA-approved as safe and effective.”
Research continues in orthopedic applications, with some studies showing potential benefits for pain management and functional improvement in conditions like osteoarthritis and tendon injuries. However, the evidence remains mixed, and long-term efficacy and safety data are still being collected.
How to Make Informed Decisions About Regenerative Medicine
When evaluating any regenerative medicine claim, patients should:
- Verify FDA approval status for the specific condition being treated
- Request published research supporting the treatment’s efficacy
- Ask about success rates and how they are measured
- Understand the risks and potential complications
- Distinguish between experimental and established treatments
- Seek multiple opinions from qualified specialists
- Consider legitimate clinical trial participation when appropriate
Any provider unwilling to answer these questions directly warrants skepticism. Patients should be particularly cautious of providers who claim their treatments are “FDA-approved” when they are actually operating under regulatory exemptions that do not require approval.
The Future of Kidney Disease Treatment: Realistic Timeline
Legitimate research continues, offering genuine hope for future breakthroughs. Current directions include artificial kidney development and drug discovery using stem cells. However, years of additional trials remain necessary before potential FDA approval.
Patients with kidney disease should continue standard care—dialysis and transplant evaluation—while research progresses. Those interested in contributing to scientific advancement can explore legitimate clinical trial opportunities through resources like ClinicalTrials.gov.
Conclusion
As of 2026, no FDA-approved stem cell treatments for kidney disease exist. This reality does not diminish the hope driving patients’ searches, but it does demand evidence-based decision-making and honest communication about what treatments are actually proven versus what remains experimental.
Patients deserve transparency about regulatory status, evidence quality, and treatment limitations. Making informed healthcare decisions requires understanding the difference between FDA approval, regulatory exemptions, ongoing research, and unproven claims.
Take the Next Step with Informed Healthcare Decisions
For those experiencing orthopedic conditions and interested in exploring regenerative medicine options, working with providers who offer transparent information about regulatory status, evidence quality, and treatment limitations is essential.
Unicorn Biosciences offers consultations for joint pain, tendon damage, arthritis, and sports injuries across locations in Austin, Dallas, Houston, Fort Worth, San Antonio, El Paso, Boca Raton, and Manhattan. The company provides PRP therapy, cell-based therapies, exosome therapy, and Bone Marrow Aspiration Concentrate (BMAC) with precision-guided injections using ultrasound or X-ray technology.
Virtual and in-person consultations are available, with same-day injection appointments when appropriate.
Contact Unicorn Biosciences at (737) 347-0446 to schedule a consultation and discuss which treatment options may be appropriate for specific conditions.
Trust providers who tell the truth about regulatory status and evidence quality.
Schedule Your Consultation Today!